Development of Disposable Balloon to Protect Aerosol Leakage of Covid-19
Thu, Nov 19, 2020-
Tags

Shinjiro Umezu
Professor, Waseda University Faculty of Science & Engineering
The coronavirus pandemic has had an immeasurable impact on the world. Classes moved online, it became difficult or impossible to visit favorite shops, and masks and hand disinfectant were not available to buy for several months. Further, the medical arena was plunged into a crisis where there were shortages of the N95 masks and other personal protective equipment (PPE) to keep doctors safe. This is the first time in modern days where people around the world are experiencing shortages of goods at the same time in this highly developed logistics era.
Meanwhile, there were news reports that engineers and researchers in the field of medical engineering are stepping up to help overcome the crisis by making face shields and swabs with 3D printers and providing them to medical institutions. These efforts were certainly not easy in the middle of an emergency.
My lab has multiple collaborative projects with medical institutions, so we have many opportunities to work with doctors on a daily basis. Facing the pandemic crisis, doctors have asked us to develop effective devices and equipment for protection against infection. After much discussion, we decided that demand was especially high for a device to prevent spray diffusion of infectious material by cough reflex during intubation and extubation (insertion and removal of a breathing tube) of patients. We believed this would be of great help to protect doctors by preventing transmission of virus from patients.
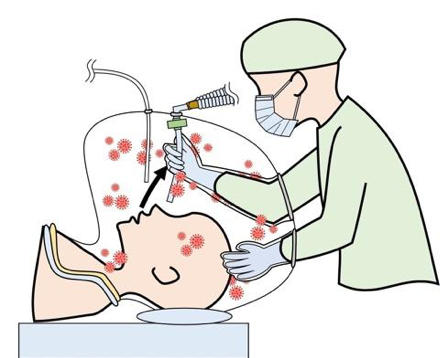
Figure 1: Extubation using BAP. Aerosols (red spots) from cough reflex are trapped inside the balloon.
Intubation is the procedure of inserting a tube into the trachea of a patient who cannot breath, securing a path for air so that a respirator can send oxygen and other gasses in and out of the lungs. The intubation tube is rigid and about 1 cm in diameter. Whereas intubation is often done under anesthesia, extubation is done when the patient is conscious and able to breathe independently without it. Therefore, extubation involves discomfort, often causing a cough reflex, sending large amounts of aerosols into the air and increasing risk of infection.

Figure 2: Suspended aerosols can be completely captured by circulation of air after procedure.
In March and April, uncertainty about the increase of patient numbers and long hours of work for fatigued doctors drew much attention. Because of shortages of personal protective equipment at the front lines of medical care, there was a need to develop and produce devices to reduce the risk of infection for doctors using inexpensive materials. In the face of this situation, a Taiwanese doctor developed an early prototype of an aerosol box and a British doctor reported results of a performance assessment [1]. However, in actual use, problems such as aerosols leaking from gaps and risk of infection during cleaning came to light.
Recognizing the need amid the pandemic, we immediately began research where we could help to solve these problems and enable practical use as quickly as possible. With the doctors who belongs to the University of Tokyo, we developed useful device, applied for patents, and wrote a research paper [2].

Figure 3: Extubation test. Visibility through transparent bag and freedom of movement during procedure was confirmed.
The device itself—called a balloon for aerosol protection (BAP)—is a bag with glove covers attached that is anchored so as to cover the patient’s head. When the cough reflex occurs, the virus will be trapped in the BAP. With the glove covers, gloved hands can move freely inside the bag and intubation tubes can be smoothly inserted and removed. Using commercially available clear bags and glove covers, it is low cost and easy to produce. The simple design means that it can be made by hand and is also suitable for industrial mass production. On top of that, being disposable eliminates infection risk involved in cleaning it, another merit.
There are other similar items and advanced technologies, but the device we are developing and improving, in addition to preventing spread of the virus, does not restrict movement of the doctor’s hands, minimizing stress on doctors. From early on, it has been forecast that the coronavirus would rage again into the winter, and we are making improvements and preparing for clinical research in time for that. We have also started work on creating a safer operating room environment.
References
[1] Barrier Enclosure during Endotracheal Intubation
New England Journal of Medicine 2020; 382:1957-1958
DOI: 10.1056/NEJMc2007589
[2] Hirose, Uchida, Umezu, “Airtight, flexible, disposable barrier for extubation”, Journal of Anesthesia, 34, 798-799 (2020).
https://link.springer.com/article/10.1007/s00540-020-02804-9
Profile
Professor Shinjiro Umezu obtained a bachelor’s degree in 2001 and a PhD (Engineering) in 2006 from Waseda University. He first became Research Associate at Waseda School of Science & Engineering in 2003, then became Special Postdoctoral Researcher at RIKEN in 2007 and Assistant Professor at Tokai University in 2009 (Lecturer in 2012), before returning to Waseda as Associate Professor in 2015 and becoming Professor in 2019.